Supporting Mental Health Treatment During and After Incarceration
November 3, 2017

MINNEAPOLIS/ST. PAUL — It’s estimated 26 percent of jail inmates suffer from mental illness or some sort of serious psychiatric distress. But a survey from the College of Pharmacy, Duluth, found many jails don’t have the infrastructure or planning in place to support those inmates, particularly upon release.
The study was published in the Journal of Correctional Health Care.
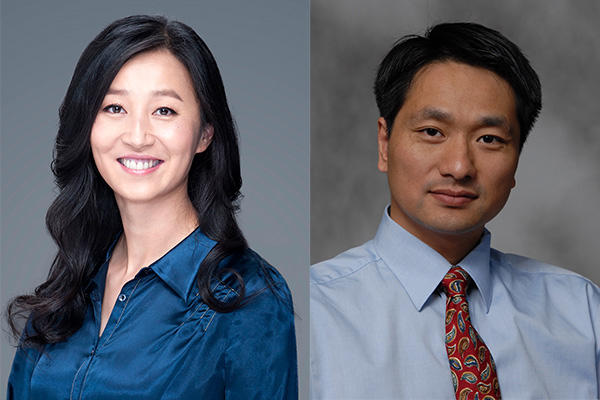
Tim Stratton, Ph.D., M.S., professor in the College of Pharmacy, Duluth, co-authored the study with Brittney Rohrer, Pharm.D., a 2017 College of Pharmacy graduate. They surveyed jails across Minnesota. Twenty six of 78 Minnesota adult jail facilities responded to the questionnaire. We spoke to Stratton who walked through some of the implications of the survey’s findings.
What’s the key takeaway from your survey?
Few Minnesota jails reported having continuum-of-care procedures in place for inmates with mental illness who are being released back into the community. Jail staff expressed desire for greater collaboration between jails, human services agencies, and community mental health providers to help support discharge planning and enhance the continuum of care for inmates who have mental illness.
Did that surprise you in any way?
Not really. Rather, the results tended to confirm what my co-author and I had both experienced in our practices. If anything was surprising, it was how great the problem appears to be across every region of the state.
How could your findings impact policy or future research?
The findings from this survey have already led to a grant from the Community Pharmacy Foundation for a telemedicine project where a community pharmacist provides medication therapy management services to inmate-patients and medication-related consults to rural county jail staff via videoconference. This project is in direct response to a need for occasional consultation with a pharmacist noted by several survey respondents. Our long-term hope is to demonstrate it would be in the best interest of the state’s taxpayers to fund this type of pharmacist interaction with county jails on an ongoing basis.
Your work points to lack of support for inmates, particularly during release and reentry into society. Why do you find it important to develop support processes and systems for people after incarceration?
Several survey respondents noted many repeat offenders who have mental illness get back in trouble following release because the offenders lack the support system necessary in the community. Such a support system is oftentimes necessary to help ensure the released inmate continues to receive their psychiatric medications, remains in treatment for their mental illness and/or substance abuse disorder and receives assistance regarding other needs such as housing, transportation, education or employment. “It takes a village” very much applies to helping released inmates who have mental illness integrate back into the community. County jails are just not equipped to provide this level and breadth of case management on their own.
According to the report, inmates often receive new mental health medications during incarceration. Does this cause additional risk or special considerations?
According to respondents, jail staff being asked to administer these newly-ordered medications may have questions about doses, indications or interactions with other drugs the inmate is receiving or tested positive for on their drug screen. Respondents noted it would be nice to have a pharmacist they could consult with about these concerns.
(Originally published by Health Talk)