
News
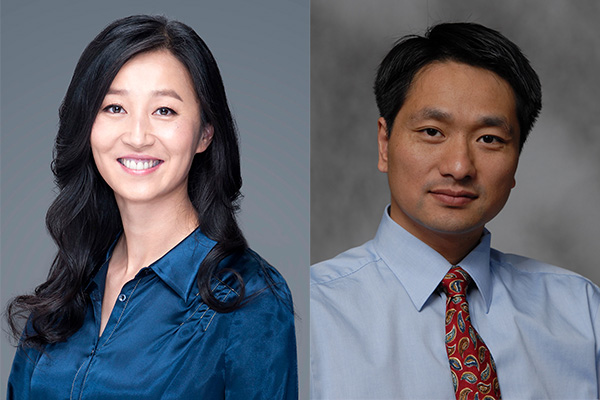
Dr. R. Stephanie Haung & Dr. Changquan Calvin Sun Named Distinguished McKnight University Professors
U.S.News & World Report rankings reflect peer assessments of program reputation

Dr. James Cloyd and graduate student Adeboye Bamgboye co-author poster
Assistant professor Shen Cheng, PhD, has joined the College of Pharmacy’s Department of Experimental and Clinical Pharmacology (ECP).

The term of service runs January 2024 through January 2028.

Developer Dr. Gunda Georg's two decades of research pave the way for this next step.

ECP alumnus Vijay Ivaturi, PhD ('10), is the new president-elect of the International Society of Pharmacometrics (ISoP). He will serve a one-year term as President-Elect prior to assuming the role of President in 2024.

Hood will start July 10; brings strong financial and strategic background
